When studying the human mind, we often crave simple and easy answers when the truth can be much more complex.
How often do you hear people say things like, “Everything about psychology is biology and genes,” or “Everything about psychology is about your thinking and beliefs,” or “Everything about psychology is your environment and upbringing.”
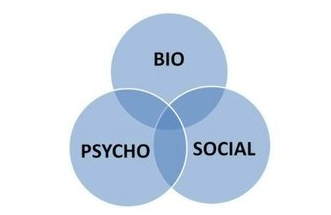
However the truth is that all of these factors influence our psychology and mental health to some degree. This is why the “biopsychosocial model” is such an important perspective when studying the human mind.
The biopsychosocial model takes into account everything that influences you and your mind. This includes…
Biological factors:
- Genes
- Health and illness
- Exercise
- Diet
- Medication and drugs
- Sleep
Psychological factors:
- Beliefs
- Emotions
- Habits
- Knowledge
- Memories
- Stress
- Perspective
Social factors:
- Family
- Relationships
- Culture
- Society and politics
- Education
- Media
- Environment
The biopsychosocial model includes all of these factors and much more. There are countless influences that come together to make you who you are – we can never narrow it down to just one thing.
So what you think of as your “self” is really a combination of all of these things at once. Understanding this can be an important part of developing self-awareness.
Of course, some of these factors we don’t have much control over (like our genes or family upbringing), but plenty of these factors we do have control over (like our beliefs and habits).
Self improvement is all about accepting the factors in your life you don’t have much control over – and focusing on the aspects of life you do have control over.
The next time you are thinking about yourself and a situation in your life, try to remember the biopsychosocial model and consider all the possible factors that have created who you are today.
Enter your email to stay updated on new articles in self improvement:
